Questions about your chemotherapy?
If you have any questions about your chemotherapy and how it is given, speak to your doctor or nurse.
You can also speak to our specialist nurses on our free Support Line.
You will have your chemotherapy at the hospital as an outpatient, so you won’t need to stay overnight.
You may be given medicines to take at home, such as anti-sickness medicine. It is important to tell your oncologist or nurse about any other medicine, vitamins or supplements you are taking before starting your chemotherapy.
Chemotherapy can be given in different ways.
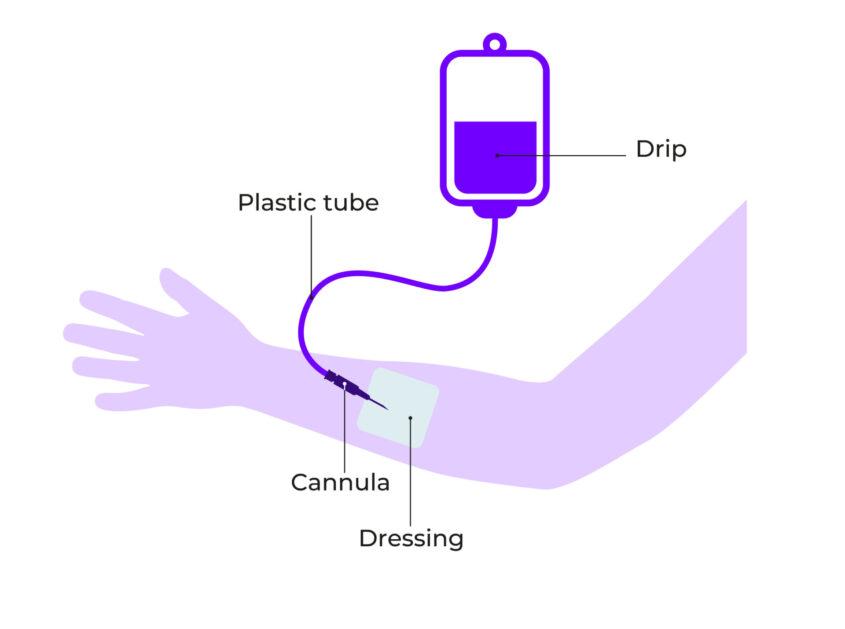
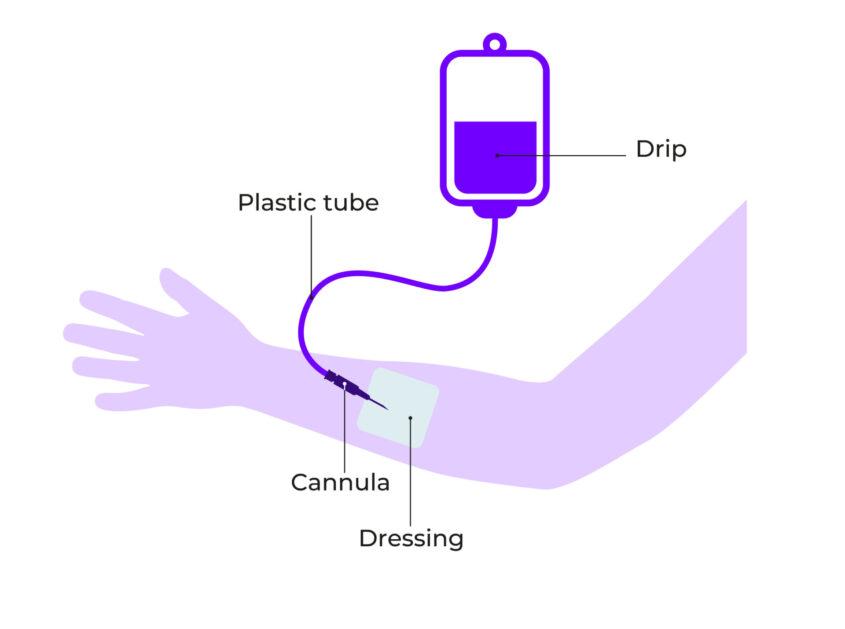
A cannula is a thin, plastic tube that is put into a vein in the back of your hand or lower arm. The chemotherapy can be given through a drip attached to the cannula, or through an injection into the cannula. The cannula will be removed after each treatment.
A diagram of a cannula:
“My mum said it felt cold when the chemo was administered into the vein via a cannula.”
You may be given chemotherapy through a central line, such as a PICC line, Hickman line or a portacath. These are long, thin tubes that are put into a vein in your chest or arm. Central lines can stay in place for as long as your chemotherapy lasts.
A diagram of a central line:
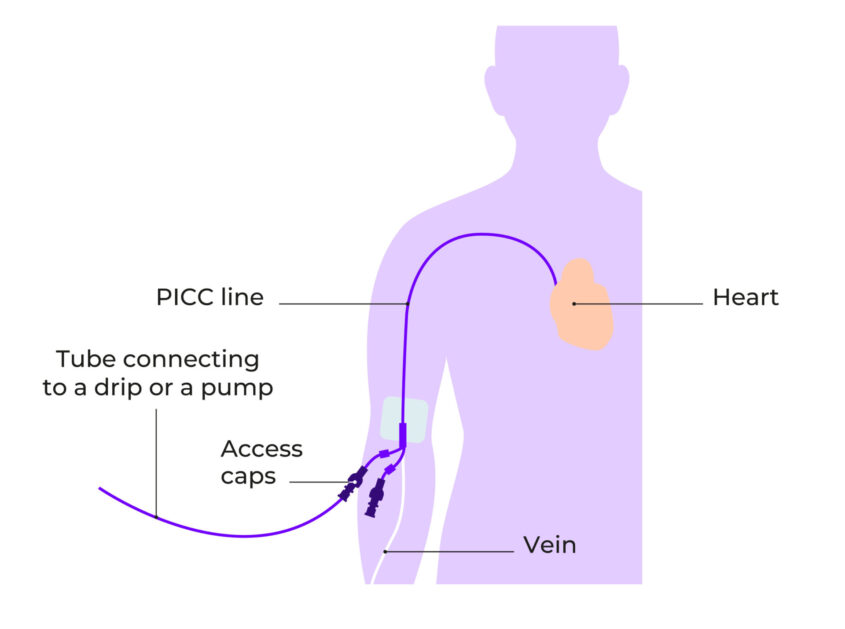
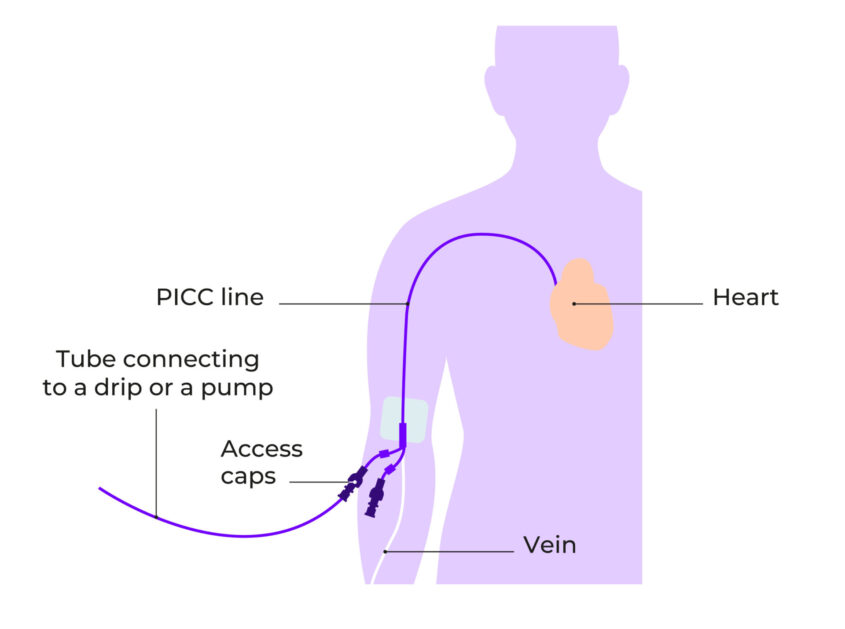
You will have a local anaesthetic to numb your chest or arm, so you shouldn’t feel any pain when you are having a central line put in.
The line will need to be flushed regularly with a small amount of liquid, even if it’s not being used. This is to make sure the line doesn’t get blocked. The area where the line goes into your body will also be cleaned and dressed when the line is flushed. You will need to keep the area clean and dry. You may be given a covering to use when showering or bathing.
Chemotherapy is normally given in cycles. A cycle is the number of treatments planned over a set time, including a break before the next cycle. The break allows your body to recover between treatments. You may have a longer break if you need more time to recover from side effects or an infection.
A cycle normally lasts two, three or four weeks, but this will depend on the chemotherapy you are having. It is common to have three to six months of chemotherapy. This will depend on how well the treatment is working and how chemotherapy affects you. Your oncologist or nurse can tell you more about this.
You will have check-ups and blood tests before each cycle to make sure it’s safe to have the next cycle. The tests check your kidneys and liver are working properly, and that your blood count has recovered enough from the last cycle.
You will also have regular CT scans to check the chemotherapy is working.
If you have any questions about your chemotherapy and how it is given, speak to your doctor or nurse.
You can also speak to our specialist nurses on our free Support Line.


Updated May 2024
Review date October 2026