Critical step towards new treatment option
Exciting new research has been published by the Pancreatic Cancer UK Grand Challenge team at Barts Cancer Institute.
Our Grand Challenge is the biggest research investment we have made to date and focuses on immunotherapy. This ambitious approach to treating pancreatic cancer aims to make the body’s own immune system fight and destroy cancerous cells.
Researchers from Barts Cancer Institute (BCI) Queen Mary University of London, have identified a protein that may be a new, specific target for the treatment of pancreatic cancer. Using this protein as a target, the team successfully used CAR T cell therapy – a type of immunotherapy – to kill pancreatic cancer cells in early stage experiments.
CAR T cell therapy is an immunotherapy that has shown great promise for the treatment of some blood cancers, but using this therapy for the treatment of solid tumours – like pancreatic cancer – has proved very difficult.
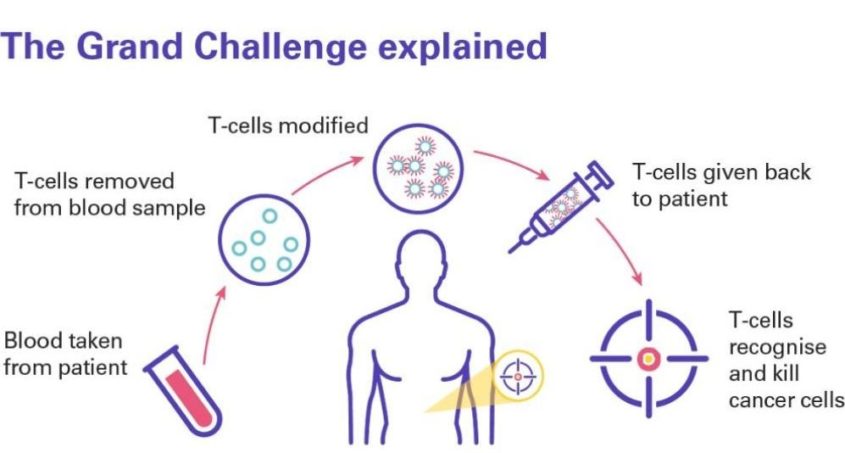
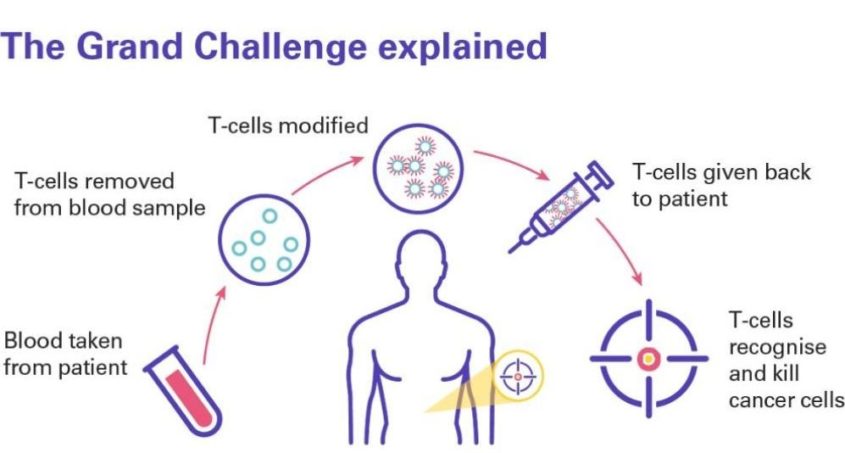
CAR T cell therapy uses immune cells (called T cells) from the patient’s blood, which help protect the body from infection and disease. T cells are taken from the patient’s blood and modified to have special proteins on their surface, called Chimeric Antigen Receptors (CAR), creating CAR T cells.
The CAR protein allows the CAR T cells to recognise a specific protein on the surface of cancer cells. CAR T cells are multiplied in the laboratory and then re-injected back into the patient where they recognise and kill cancer cells that have the target protein on their surface.
The protein identified by the team in the study, published in Clinical Cancer Research and funded by Pancreatic Cancer UK, is called CEACAM7 and may be a safer treatment target for the development of therapies against the most common type of pancreatic cancer (pancreatic ductal adenocarcinoma – PDAC).
By using a special technique called immunostaining, the team looked at pancreatic cancer tissue samples against normal tissues taken from other parts of the body. CEACAM7 could be found in the pancreatic cancer samples, but not in the normal tissues, which suggests that this protein could be an ideal target for developing CAR T cells against pancreatic cancer.
Our Head of Research, Chris Macdonald said:
“For the first time, a distinct and specific target protein for pancreatic cancer cells has been identified and, crucially, the brilliant team at Barts have shown that by focusing on it, they can destroy the cancer without damaging healthy tissue. This has never been done before in pancreatic cancer and marks an important step towards a desperately needed new treatment option, which could be both more effective and have fewer side-effects for patients.”
This is an exciting development. Finding that CEACAM7 allows us to kill pancreatic cancer cells specifically with CAR T cells, while having no significant toxicity in non-tumour tissues, gives us hope that this strategy could be effective in the future. It is also possible that other types of immune-based therapies could be directed to CEACAM7 for the treatment of pancreatic cancer

